- Home
- Skin Cancer
Thinly invasive melanoma
Understanding Your Melanoma Diagnosis: Thinly Invasive Melanoma (< 1mm Breslow Thickness)
Dr. Chris Irwin
The Skin Doctor
Being diagnosed with melanoma can be scary, but the good news is that the type of melanoma you have, even though it is invasive, is still early-stage and will most likely be completely cured by simple surgical removal with margins. This handout explains thinly invasive melanoma —and why it usually does not require additional tests like lymph node biopsies or body scans. We’ll also discuss what to expect next and how these early melanomas are managed in a patient-friendly way.
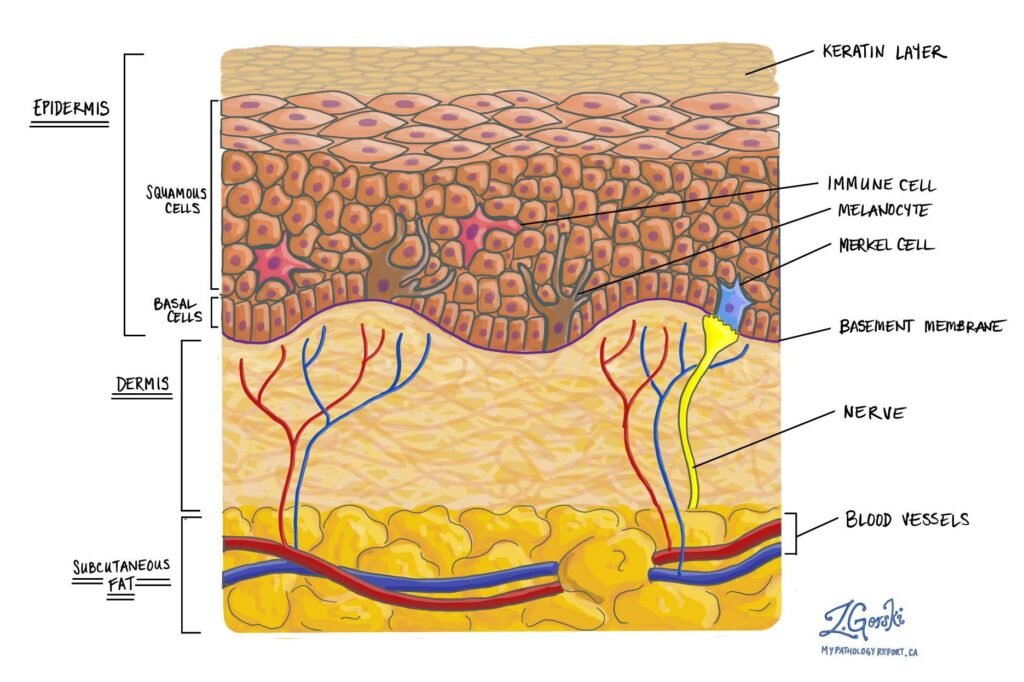
Figure 1. Histological diagram of an invasive melanoma
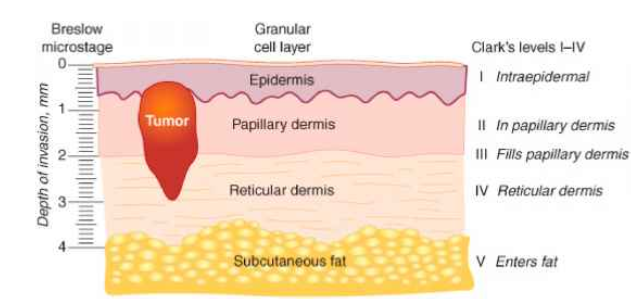
Figure 2. Explanation of Breslow thickness (credit : Steven Chen
If your report says you have an invasive melanoma with a Breslow thickness < 1mm, this is often called a “thinly invasive melanoma” and corresponds to an early Stage I melanoma. “Invasive” simply means the melanoma did grow deeper than the epidermis into the second layer of skin (dermis) – breaking through the strong canvas layer called the basement membrane or “dermo-epidermal junction”, but in this case only slightly.
Thinly invasive melanoma is more serious than in situ melanoma because there is a low chance of spread through the body. How serious an invasive melanoma is depends on several variables. The primary “badness” marker is the breslow thickness.
Breslow thickness is a measurement in millimetres from the top of the skin (technically the granular layer of the epidermis) to the deepest point of invasion by the melanoma. Let’s put this into perspective though, 1mm is the same thickness as a grain of sand. If you have a melanoma less thick than a grain of sand, the most likely outcome if you are treated properly is that everything will be completely fine.
Figure 2. Explanation of Breslow thickness (credit : Steven Chen https://x.com/DrStevenTChen/status/1345490623822921728)
The reason why we care the most about the Breslow thickness is it is the main marker for how likely a melanoma has spread to regional lymph nodes (like in the armpits or groin) – or further.
In general the risks for spread for a thinly invasive melanoma are really low – less than 5%.
Other risk factors (that will be on the histology report from the lab) that make spread more likely are:
- ulceration
- mitotic rate >1
- Clark level IV or V (ie extending into the reticular dermis or into fat – but of course this is very unlikely in melanoma <1mm thick!)
- Lymphovascular invasion
Histology reports are very complicated and have a whole bunch of other words on them. If you have any questions about the specific words feel free to ask during your consult. In the vast majority of cases though, anything other than the breslow thickness, and the other risk factors discussed above doesn’t really alter management.
Do I need further scans or tests to make sure it hasn’t spread?
In general, no. For most patients with thinly invasive melanoma, the risks of the scans or tests outweigh the benefit they provide.
Current guidelines in Australia state that If a melanoma has a breslow thickness 0.7mm-1mm AND has any of the risk factors above (ulceration, mitotic rate >1, Clark level IV or V or Lymphovascular invasion), we discuss the role of Sentinel Lymph Node Biopsy (SLNB). (https://melanoma.org.au/wp-content/uploads/2021/11/Clinical-Brochure-Sentinal-Node-Biopsy.pdf)
In basic terms a SLNB is a procedure to see whether the closest lymph node contains any melanoma cells that have spread from the skin. It requires a general anaesthetic (being put to sleep) and has some significant risks associated with it. The overall risk of a complication from SLNB is around 11.3% (https://cinj.org/sites/cinj/files/documents/Complications%20of%20sentinel%20lymph%20node%20biopsy%20for%20melanoma%20-%20a%20systematic%20review%20of%20the%20literature.pdf). While it is important to consider this procedure if your risk of spread is >5%, we don’t recommend this procedure for most low risk thinly invasive melanomas, as we are more likely to harm you than help you with the procedure.
Key facts about thinly invasive melanomas:
- Low risk of spread: Thin melanomas have a very low risk of metastasis as well, though slightly higher than in situ. The risk of cancer cells having spread to lymph nodes or beyond is under 5% for melanomas thinner than 0.8 mm, and in the range of about 5–12% for those between 0.8 and 1.0 mm
- Surgery is the main treatment: Just like melanoma in situ, the first step is a wide local excision surgery to remove the melanoma with a safety margin of normal skin. Typically, a margin of 1 cm (about 0.4 inches) of normal skin is taken for melanomas up to 1mm thick (per guidelines) to ensure clear margins
- Sentinel lymph node biopsy usually not needed: Because the chance of spread is so low, additional lymph node testing isn’t usually recommended for these thin melanomas. In fact, medical guidelines do not recommend a sentinel lymph node biopsy (SLNB) for most thinly invasive melanoma
- No routine scans needed: Just like with melanoma in situ, full-body imaging scans (CT, PET, etc.) aren’t done for a thin melanoma that shows no signs of spread. The chance of any scan finding melanoma in other organs at this early stage is extremely low, so doctors avoid exposing you to unnecessary radiation or causing anxiety from false alarms.
- Excellent prognosis: The outlook for thin melanomas is overwhelmingly positive. Survival rates are above 95–99% at 5 years for Stage I melanoma patients
- The vast majority of people in this category remain cancer-free after treatment. You will still need regular skin checks (often every 3-6 months for the first two years) to watch for any new melanomas or changes, but the melanoma you had is very unlikely to come back after proper removal.
Takeaway: Thin invasive melanomas (<1mm) are early-stage skin cancers with a very low risk of spread. Treatment is minor surgery to remove it with a margin. Additional procedures like lymph node biopsy or body scans are usually not done because they are not likely to find anything in such low-risk cases
Follow-Up and Outlook
Your prognosis is extremely good. Both melanoma in situ and thin invasive melanomas have high cure rates after proper removal – meaning the vast majority of patients remain alive and well, with no recurrence of melanoma. Many experts would say you are likely cured at this point. Here’s what to expect moving forward and some tips for peace of mind:
- Regular Skin Checks: You will need periodic skin checks and reviews with your skin doctor. Typically, for a thin melanoma, the schedule might be every 3-6 months for the first couple of years, before moving to a long term 6-12 month review cycle.
- These visits are to ensure no new melanoma (or other skin cancers) develop and to catch any changes early. Self skin exams at home monthly are also a good habit – your doctor can teach you how to examine your moles and what to look for.
- No Routine Scans or Blood Tests: As discussed, you won’t be undergoing regular CT/PET scans or blood work for melanoma markers, because there’s no indication to do so. Try not to be alarmed by the lack of testing – it truly is a positive sign about your prognosis. Of course, if you develop any new symptoms (for example, a new lump in your groin/armpit, unexplained persistent pain, etc.), inform your doctor. They will investigate appropriately. But such scenarios are not expected given how early your melanoma was.
- Scar Care: You will have a scar from the surgery. Keep it clean and protected from the sun as it heals. Over time (months to a year) it will fade and soften. Your doctor can advise on great dressings like mefix, scar creams or silicone gel sheets if needed. Most patients find the scar becomes a minor cosmetic issue, especially compared to the relief of being cancer-free. The more care you take for your scar in the first 3-6 months the far better the long term scar will look!
- Sun Protection: One of the best ways to prevent future skin cancers is to practice good sun safety. That means using sunscreen (SPF 50) on exposed skin daily and reappying every 2 hours whenever outside, wearing hats and protective clothing.
- Peace of Mind: It’s normal to feel anxious after a cancer diagnosis, even one as low-risk as this. Remember that your melanoma was caught at a very early stage. If you find yourself worrying a lot, consider discussing these feelings with your doctor. Sometimes connecting with a counselor or a support group of melanoma survivors can be helpful. Knowing others have gone through the same thing and are doing fine can be very helpful.
